What's Inside
Type 1 diabetes is an autoimmune disease. This can cause your blood sugar levels to become too high.
Overview Of Surgical Treatments
A cure for type 1 diabetes is not possible because it is an autoimmune disease, but there are several treatment options available to manage the disease.
However, surgery can be used in some cases of type 2 diabetes to try to improve blood glucose control. In some cases, surgery may be used as a last resort when other treatments have failed.
Some Surgical Treatments Include:
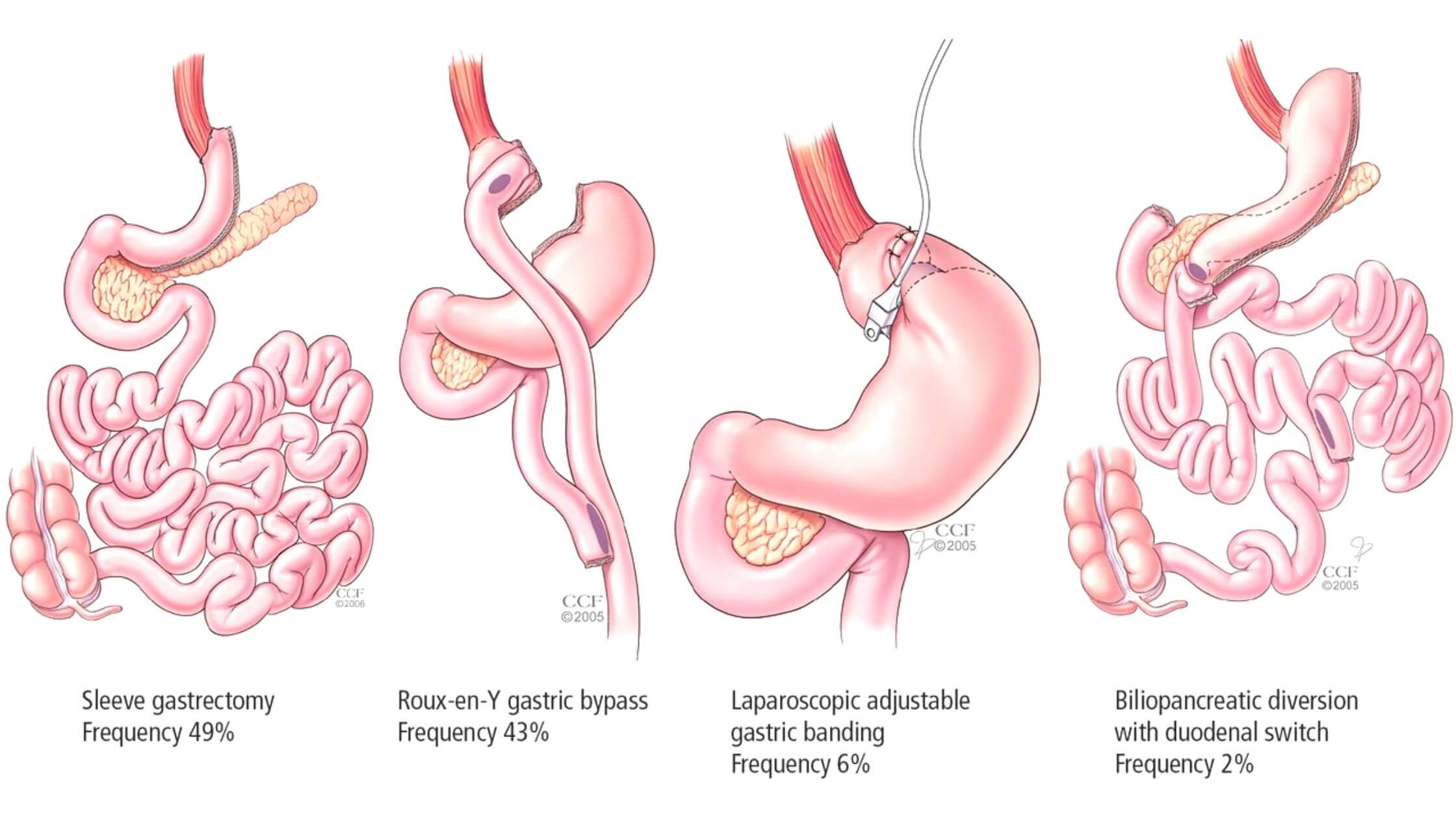
Gastric Bypass
This procedure changes the size of your stomach so that you feel full sooner and eat less food overall. It also reduces the absorption of calories from food by bypassing much of the small intestine and rerouting nutrients into a small pouch formed by surgical removal of a section of the stomach and shortening of the small bowel.
Biliopancreatic Diversion (BPD)
This procedure also changes how food moves through your digestive tract by removing most of your stomach and intestines so they do not absorb food properly anymore leaving behind only a small pouch inside the abdomen that collects fluids that come from digestion.
Adjustable Silicone Gastric Banding (ASGB)
This type of restrictive surgery includes a silicone band around the upper part of your stomach that can be inflated or deflated depending on how much food you eat.
Sleeve Gastrectomy
During this procedure, about 85 percent of your stomach is removed so only a small tube-shaped pouch remains to leave you with a smaller stomach than before surgery.
Pancreatic Islet Transplantation
A surgical procedure for people with type 1 diabetes involves transplanting pancreatic cells (islets) into the liver, where they will produce insulin. This procedure has been done successfully in clinical trials, but it is not available outside of research studies at this time.
Duodenal Switch
In this surgery, part of the stomach is removed so that food empties into a small pouch rather than the rest of the stomach. The small intestine is then connected directly to this pouch instead of being connected to an opening in the stomach — making it easier for food to pass through and reducing nausea after meals.
Vertical Sleeve gastrectomy
This surgical procedure removes most of your stomach, leaving behind a thin tube-like structure that creates less room for food to be stored and digested before it leaves the body through digestion. Vertical sleeve gastrectomy may improve blood sugar control in some people with type 2 diabetes who lose significant amounts of weight after surgery.
Preparing For Surgery When You Have Diabetes
If you have diabetes, it’s important to discuss your condition with your health care team before surgery.
You may need to change your insulin or blood sugar level before and after surgery. This is done by careful monitoring of your blood sugar. You may also need to take special steps to prevent hypoglycemia (low blood sugar).
Header text
- Before surgery, you should eat a meal that includes carbohydrates (such as fruit or vegetables) and protein, such as a sandwich or yogurt. This meal should be eaten at least two hours before the surgery starts time.
- During surgery, you will be given an IV (intravenous) line that delivers fluids and medications directly into your bloodstream. The IV line can also be used to give insulin injections if necessary.
- After surgery, you will be monitored closely in the recovery room for signs of high or low blood sugar levels.
After surgery, you may also need to take some steps to prevent complications:
Check your blood sugar levels frequently. This is important because the body uses sugar differently after surgery than it does when there are no surgical wounds or other injuries. If your blood sugar level is high, this can lead to tissue damage and infection.
Take insulin or oral diabetes medications as prescribed by your doctor. This will help keep your blood sugar level stable during recovery from surgery and reduce the risk of infection.
Eat a healthy diet that includes plenty of protein and fiber and limits fat intake as much as possible. Protein helps rebuild muscle tissue, while fiber helps prevent constipation and diarrhea — both common issues after surgery. Fiber also may help prevent spikes in blood sugar after eating a meal.
Type 1 Diabetes And Surgery Risks
They may also need to take other medications to treat complications from high blood sugar levels, such as high cholesterol and high blood pressure.
People with type 1 diabetes have an increased risk of developing health problems during and after surgery, including:
- Hypoglycemia (low blood sugar) during or after surgery
- Infection
- Blood clots
- Damage to nerves in the legs (peripheral neuropathy).
Laparoscopic Surgery For Diabetes
Laparoscopic surgery for diabetes is a surgical procedure that opens up the abdomen to treat diabetes. This type of surgery involves making tiny cuts in your belly and inserting a tube with a light on it into your stomach.
The procedure can be done as an open operation or by using laparoscopy, which uses small incisions.
The surgeon makes an incision in your belly button or navel (laparoscopic). The surgeon then inserts a small instrument that has a camera lens attached to it through one of the incisions. The surgeon views the image on a television monitor and operates through other small incisions.
The surgeon may also use instruments that are inserted through other incisions to remove parts of your pancreas, liver, stomach, duodenum (the first part of your small intestine), gallbladder and spleen if they’re diseased or damaged.
Pancreas Transplant For Type 1 Diabetes
A pancreas transplant is a treatment option for people with type 1 diabetes who don’t produce enough insulin or can’t maintain their blood sugar levels.
Pancreas transplants are done as part of a kidney-pancreas transplant, where the donor pancreas is placed in the lower abdomen. Or it can be done separately as a single organ transplant.
The most common reason for needing a pancreas transplant is chronic rejection (when your immune system attacks the new organ). Chronic rejection occurs when you have an incompatible blood type or antibodies against foreign tissue, such as that from an organ donor. Chronic rejection is more likely in older people and those who have had previous transplants or other abdominal surgeries.
A second reason for needing a pancreas transplant is diabetes complications such as blindness, kidney failure, or heart disease caused by high blood sugar levels over many years.
Conclusion
If you have type 1 diabetes, you’re not alone. Everyone with type 1 can expect to face surgery challenges in the coming years as their disease progresses.
Those who actively check glucose levels and follow their doctor’s advice will be likely to stay healthy, but the need for management will only grow over time.
When questions arise, it’s important to consult a health professional to make sure that management plans are appropriate and effective.

